By Neil Westphalen*
A PDF version of this article can be dowloaded here:
Endnotes: Formatting problems mean the endnotes cannot be added to this article but can be downloaded as a Word document using the following link:
Introduction
On 05 February 2019, Chief of Navy (CN) anticipated a busy year, balancing Navy’s current commitments with emerging activities in the southwest Pacific and southeast and northeast Asia. The ensuing need for more ships at sea accounts for his imperative to improve Navy recruiting and retention.2
It is therefore of concern that the proportion of Permanent Navy (PN) members with at least one medical restriction has increased four-fold since the mid-1990s, while those deemed medically unsuitable for sea for more than 28 days has nearly tripled. Furthermore, the current compensation claim rate among current and ex-serving Australian Defence Force (ADF) – including Navy – members could be five times the worst civilian serious worker’s compensation claim rate, while their per capita cost to the Department of Veteran’s Affairs (DVA) could be twice the civilian median cost. A recent study also indicates that up to 90 per cent of Army (hence by extension Navy and Air Force) work-related injuries and illnesses are not being reported.
Career and other individual impacts aside, this situation suggests that, besides improved recruiting and retention, CN’s operational imperatives also demand better prevention, monitoring, early intervention, treatment and rehabilitation for avoidable illnesses and injuries. The fact that such measures also reduce compensation costs explains why many civilian organisations consider them best practice,3 and they will be essential if a Productivity Commission proposal to charge the ADF premiums for work-related illnesses and injuries comes to fruition.4
These measures are not new to the military setting. In 1940, medical officer and Gallipoli veteran Colonel Arthur Graham Butler5 described how military health services have not one but three missions, with one assuming priority depending on circumstances:
* Alleviate suffering, by providing treatment services.
* Enable operational capability, by keeping members medically, dentally and psychologically suitable for employment and deployment.
* Enable their eventual return to the civilian community, with respect to their service-related illnesses and injuries.6
As the latter have no comparable remit, military health services are profoundly differentiated from their civilian counterparts by the second and third of these missions. Yet, the aforementioned health status of Navy personnel indicates the extent to which the functions and roles of the ADF’s health services, and their enabling Fundamental inputs to (health) Capability (FiCs),8 are currently focused only on providing treatment.
This disparity stems from longstanding misperceptions by ADF commanders, Defence health personnel and other stakeholders,9 regarding the non-treatment-service-related reasons as to why military health services exist. As a result, the current ADF health service delivery model can be summarised as an attempt to control excessive costs by restricting perceived over-servicing in the base or ‘garrison’ setting,10 while enabling the non-clinical logistic and administrative requirements of deployable treatment services.11
This paper asserts that a key contributor to these misperceptions pertains to a lack of enduring military doctrine regarding for whom, where, why, how and therefore what health services are required – besides clinical care – for ADF operations in general, and maritime operations in particular.12
Australian military doctrine overview
The ADF’s elemental doctrinal reference is Australian Defence Doctrine Publication–D (ADDP–D).13 This document describes how military doctrine is informed by lessons over time, as to how military forces should be directed, mounted, commanded, conducted, sustained and concluded, in support of national policy.14 Although it is informed by the latter (via the extant Defence White Paper15 among other references16), military doctrine is more enduring. While it is authoritative, the fact that military doctrine is not immutable means its application still requires careful judgement.17
In addition, the Services each have their own references that maintain an interdependent association with ADDP–D, while describing the elemental doctrinal aspects of the maritime, land and air environments.18 They are:
* Navy: RAN Doctrine 1: Australian Maritime Doctrine (AMD)19
* Army: Land Warfare Doctrine (LWD) 1 – The Fundamentals of Land Warfare20
* Air Force: Australian Air Publication (AAP) 1000-D – The Air Power Manual21
These documents guide each Services’ subordinate doctrinal references. Navy’s include Australian Maritime Operations (AMO),22 which describes Navy capabilities, limitations and organisation, and Australian Maritime Logistics Doctrine (AMLD),23 which explains how Navy conducts logistics support for maritime operations.
The ADF / Navy health references within each of these documents are as follows:
* ADDP-D refers to health services as a command responsibility24, a logistic function,25 and a force protection measure.26
* AMD notes that health services will be provided from the Canberra Class Landing Helicopter Docks (LHDs) for amphibious operations.27 It mentions historical examples,28 refers to battlespace health threats,29 and peacekeeping medical team operations.30 It notes Command’s health responsibilities,31 and to effective medical treatment as a major morale factor as an enabler of sea power.32
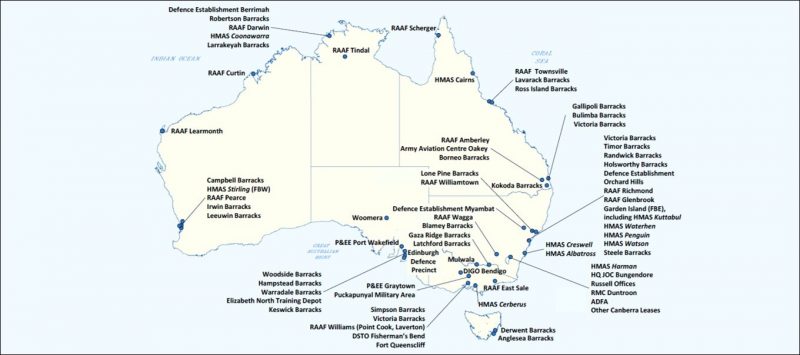
* AMO refers to delivering Navy health training,33 Command’s occupational health and safety responsibilities,34 health and quarantine obligations per the United Nations Convention on the Law of Sea (UNCLOS) 1982,35 and health care for Humanitarian Aid / Disaster Relief (HA/DR) operations.36 It also lists the Joint Health Command (JHC) health facilities at each Navy shore establishment.37
* AMLD replicates AMO and ADDP-D by referring to health support as a logistics function,38 and to healthy workplaces as a warship endurance enabler.39
Hence, Navy’s doctrinal health references are fragmented and incomplete. None specifically describe how the missions of its supporting health services extend beyond providing treatment services, to also enabling maritime operational capability and facilitating civilian re-integration. Neither do they articulate the elemental functions and roles that its enabling health services need to perform in order to conduct these missions, or the FiCs they require from the rest of Navy and Defence for them to do so.
The scope of occupational health
This paper also contends the aforementioned misperceptions include the scope of occupational health services in general, and of occupational and environmental physicians (OEPs) in particular. For example, the current JHC ‘garrison’ health contract excludes OEPs as part of their multidisciplinary rehabilitation teams, even though they are not only trained to set the pace and direction of workplace-based outpatient rehabilitation, but also to negotiate with employers and other stakeholders to achieve optimal return-to-work outcomes.
Contrary to these misperceptions, OEPs have the medical specialist professional qualities to undertake both clinical and population-based practice, with respect to the chemical, physical, biological, psychological, emotional, environmental and psychosocial hazards related to work-related illness and injury, via:
* Assessment and treatment of work-related illnesses and injuries.
* Conducting fitness and return to work assessments.
* Providing specialist workplace rehabilitation advice.
Furthermore, OEPs have a preventive clinical role with respect to:
* Conducting workplace hazard assessments.
* Undertaking critical appraisal of information regarding the relationships between workplace hazards and employee health.
* Conducting research regarding the relationships between workplace hazards and employee health.
* Working with governments, regulators, employers, workers and other stakeholders to ensure positive health outcomes for both workers and employers.
* Providing specialist advice regarding the relationships between medicine and workplace health, safety rehabilitation and compensation legislation.
* Providing specialist health advice regarding workplace environmental hazards that may be affecting the general community beyond workplaces.
* Providing specialist workforce health promotion advice.40
This paper therefore asserts that the skills and expertise of OEPs are directly germane to:
* The health services required for current Navy members, and the vocational rehabilitation and compensation processes for current and ex-Navy members.
* The doctrinal basis for health services, with specific reference to maritime operations.
Aim
The aim of this paper is to explain the need for, and to outline some of the elements of, an enduring doctrinal reference regarding health support for Australian maritime operations.
Scope
It is hoped this paper will lead to a document comparable to AMO and AMLD that describes:
* the elemental functions and roles required of Navy’s enabling health services, for them to undertake the missions per Butler in support of maritime operations, and
* the FiCs required by these health services from Navy and Defence, for them to perform these functions and roles.
This paper will also explain why this reference ought to be based on a best-practice occupational health systems model.
In addition, it is hoped such a reference will inform future Navy and ADF military doctrine.
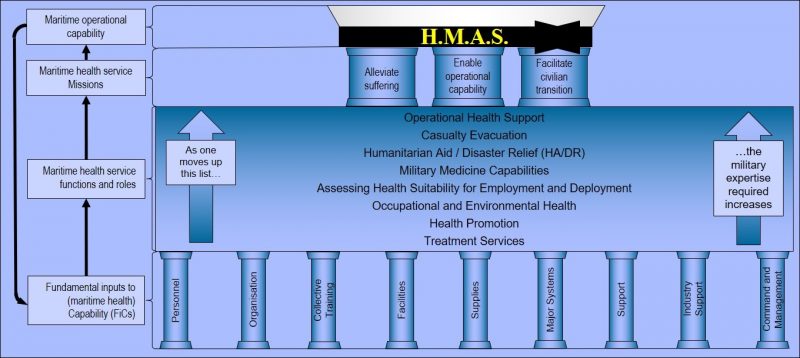
Figure 1 forms the basis of a future maritime health doctrine reference. It summarises the relationships between maritime operational capability, the enabling health services’ missions per Butler, their functions and roles to conduct these missions, and their enabling FiCs from Navy and Defence.
Methodology
Simon Sinek’s ‘Golden Circle’ explains why organisations should base their primary reason for existence firstly on ‘why’, followed by ‘how’ and then ‘what’.41 Figure 2 shows how the size and scope of any population’s health services (Sinek’s ‘what’) can be derived from:
* the target population’s demographics (the ‘who’).
* The locations in which it lives and works (the ‘where’).
* What it does (Sinek’s ‘why’).
* The ways in which ‘where’ and ‘why’ affect its health services (Sinek’s ‘how’).

Navy’s population demographics: the ‘Who’
As per Figure 2, this paper asserts that ascertaining the size and scope of military health services should begin with the target population’s demographics.
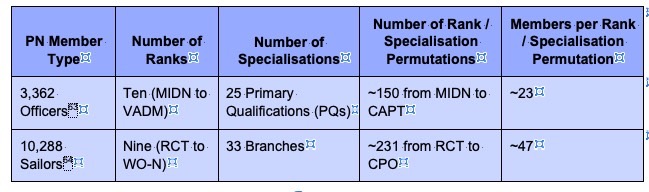
Numbers. In 2017-18, Navy had 13,818 full-time members,43 which is scheduled to increase to 14,763 by 2020-21.44
By comparison, the ADF had 58,475 full-time members,45 including 2,404 who were force-assigned to Joint Operations Command (JOC), 46 while the Australian Public Service comprised 136,175 permanent and 14,419 non-ongoing (contract) employees.47
More broadly, the three largest Australian private employers were Wesfarmers (217,000),48 Woolworths (201,000)49 and Rio Tinto (47,000).50 Unlike the ADF however, these employers do not provide clinical health services, while most of their employee medical conditions do not require the same level of consideration of their work capacity, with respect to operational capability.51
While the ADF therefore constitutes one of the largest workforces in Australia, only about 25 per cent are PN. As the ADF does not routinely provide health services for reservists, this paper assumes Navy requires health support for 14,000 members. This population is comparable to Nelson Bay NSW (population 13,967), Warragul VIC (14,274), Warwick QLD (13,860), Broome WA (13,984), Port Lincoln SA (14,062), and Ulverstone TAS (12,032),52 or about half the Qantas workforce (27,000).53
Age. By definition, all PN members are over 17 years old and virtually all are under 65, compared to 66.0 per cent of the Australian civilian population.54 Furthermore, 22 per cent of PN members were 17- 25 years old in 2018, compared to 12.8 per cent of the civilian population who were aged 15-25 at that time.55
The fact that the ADF does not provide care for cadets, family members or veterans therefore means that Navy is not only a workforce population, but a young workforce population.
Gender.56 2,935 PN members (21.5 per cent) were female in 2017-18,57 compared to 47.0 per cent of the Australian civilian workforce.58 Women are planned to reach 25 per cent of the Navy workforce by 2023.59
Health Standards. All ADF entrants undergo a health assessment process that includes a comprehensive health questionnaire and physical examination by medical and dental practitioners, as well as extensive psychological testing.60 As currently serving members should also meet the relevant retention health standards, Navy probably has one of the most highly medically-selected workforces in Australia.
Workforce Complexity. Navy presently has 50 PN and ten ANR entry-level jobs.61 As every officer and sailor rank can have up to ten skill-level-based pay rates,62 Figure 3 gives a notional 2.3 officers per rank per PQ per pay rate, and 4.7 sailors per rank per branch per pay rate. While these figures clearly do not reflect the actual PN workforce, they still indicate why the smaller PQs / branches often lack depth regarding their skills base.
Moreover, over 1,814 Navy members (13.2 per cent) were under training in 2017-18,65 a proportion that is probably higher than most civilian employers. Navy also conducted nearly 2000 courses in 2017, many of which were for its trained force, including those at sea.
Navy therefore probably also has one of the most complex workforces in Australia.
Duration of Service. In 2015, the median duration of service for Navy members was seven years, while 38 per cent had served less than five years.66 While the average duration of civilian employment is 3.34 years,67 this figure does not consider Navy’s posting cycle (see below).
These figures confirm Navy has a high-turnover workforce.
Navy’s population locations: the ‘Where’
As per Figure 2, ascertaining the size and scope of health services should then consider the target population’s geographic distribution and mobility.
Population Distribution. About two-thirds of the Navy workforce (9300 members) are posted to 14 shore establishments, or to over 40 non-Navy ADF bases throughout Australia (Figure 4).68 The remaining third (4700) are distributed among 50 seagoing Fleet units and non-commissioned vessels.69 When not overseas the latter are alongside one of five homeports, two of which are in Sydney.
Up to 800 seagoing Navy members are force assigned to JOC,70 while the remaining 3900 undertake Navy-led activities in Australian waters, as well as regional and other deployments (see below). While the turnover between being alongside and at sea varies considerably, an average of one third (1600) who are physically at sea at any one time appears a reasonable estimate.71
Even for those who are not posted to ships, the Navy workforce is therefore widely distributed across Australia.
Workforce Mobility. All PN members participate in posting cycles of two to three years’ duration (hence at least 4700 planned postings per year), to which can be added unplanned postings for compassionate, disciplinary, medical and other purposes. Although many shore postings are ‘back-to-back’, this is not always possible for Service and career development reasons (see below).
Hence, even without deploying, the Navy workforce is also exceptionally mobile.
Navy’s operational environment: the ‘Why’
As per Figure 2, ascertaining the size and scope of health services should then consider why the target population exists.
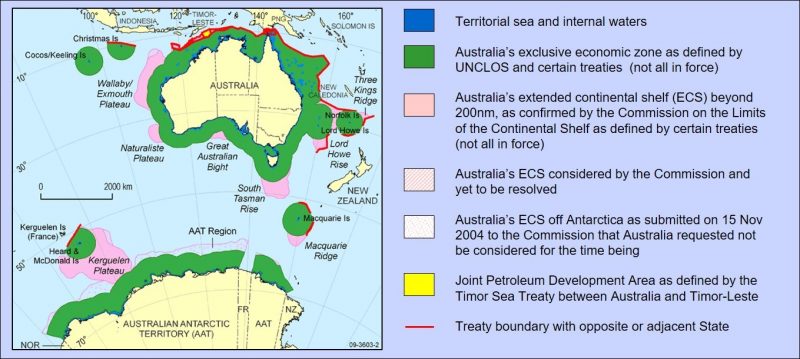
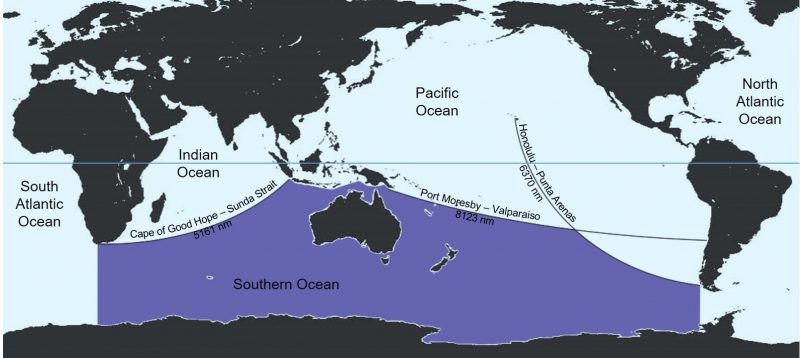
Australia’s Strategic Geography. AMD states the global ocean is huge: at 362 million km2,73 it covers 70% of the Earth’s surface74 and can fit Australia 47 times.75
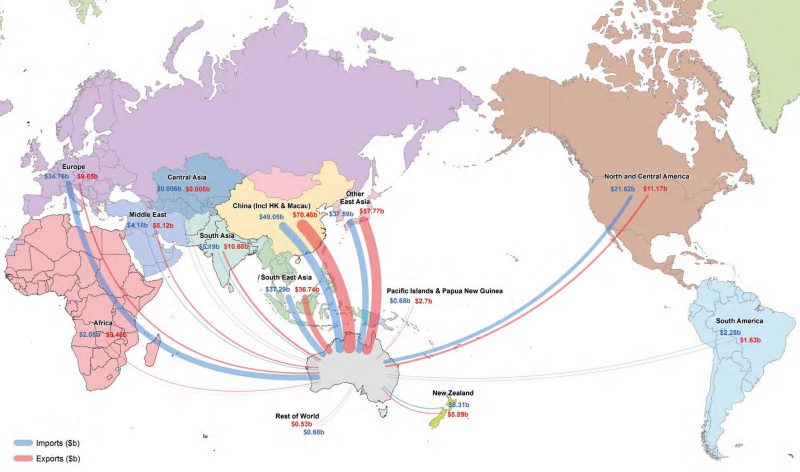
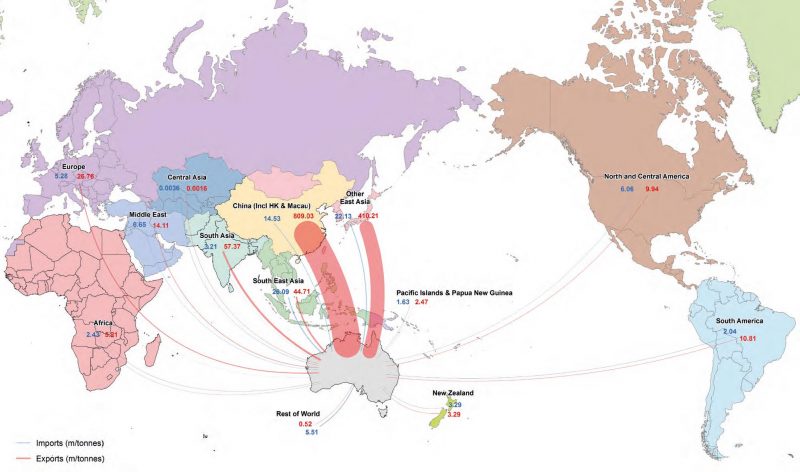
The global ocean also connects every land mass on Earth, thereby enabling the prosperity upon which Australia’s national interests are based: while Australians routinely travel by air, over 75 per cent of their exports and imports by value (about $300 billion in 2016),76 and 99.9 per cent by weight, still moves by sea.77
Australia also has several maritime jurisdictional areas (Figure 5). These total 14 million km2 (nearly twice Australia’s land area), which makes them among the largest in the world. Their climates vary from the intense heat and humidity of the tropics, to the extreme cold and huge seas of the sub-Antarctic.78 In 2013-14, these areas contributed $53.8 billion to the Australian economy.79
AMD therefore notes distance as the key feature of Australia’s strategic geography.
In addition, AMD notes that nearly all shipping between Australia and its major trading partners passes through several choke points that can be blocked by potential adversaries.80 Figure 6 shows that nearly 80 per cent of Australian seagoing exports and over 60 per cent of its imports by value pass through the northern archipelago, while Figure 7 shows this equates to 90 per cent of its exports and nearly 65 per cent of its imports by weight.
Furthermore, Figure 8 shows that potential adversaries can also identify (and hence target) ships in the Indian and Pacific Oceans as en-route only to or from Australia or New Zealand from some considerable distance. The boundary that makes this possible is referred to as the ‘Sandison Line’.81
AMD also notes that:
* Although ships move at only one-thirtieth the speed of aircraft, they can carry thousands of times the payload.86 Ships can also remain on station for weeks or months,87 while aircraft can only do so for a matter of hours.88
* For most of northern Australia, the northern archipelago and the south Pacific, the lack of road, rail or air alternatives means that the sea either provides the sole means of access, or is the only way to move large volumes of people and cargo.89
Hence perhaps more than any other nation, Australia’s area of regional interest constitutes a maritime-littoral environment.90
In summary, Figures 5-8 demonstrates the reasons why Australia’s use of the sea to further its prosperity means that its national interests are global. They also explain why Australia has a Navy for reasons beyond simple territorial defence.
Australian maritime operations: the ‘How’
As per Figure 2, ascertaining the size and scope of health services should then consider what the target population does.
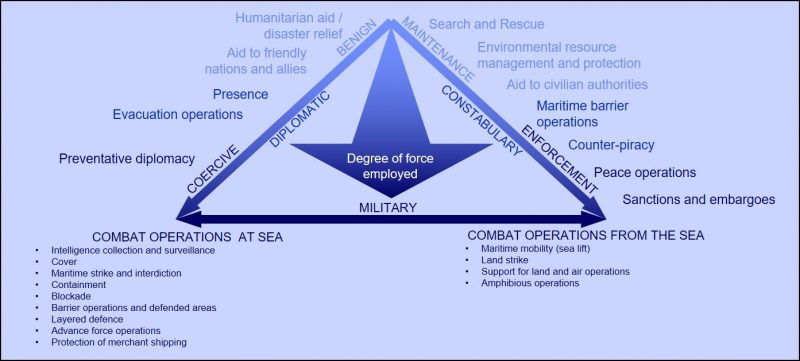
The Spectrum of Maritime Operations. AMD describes how maritime operations can influence events ashore.91. Figure 9 shows how the conditions that create and sustain conflict produce multiple contingencies within a spectrum of operations that can be divided into three parts: peacetime operations, operations other than war, and warlike operations.92
Figure 10 illustrates the means by which the spectrum of maritime operations per Figure 9 can be conducted.93

Peacetime Operations. AMD describes how Navy is employed in peacetime to preserve and protect Australia’s enduring values and interests.95 To these ends, Navy has undertaken numerous emergency relief operations,96 and aided civil authorities,97 while maintaining surveillance patrols of the Australian maritime domain (Figure 5),98 and conducting multiple maritime border protection and related law enforcement activities.99
Operations Other Than War. AMD describes ‘operations other than war’ as military activities short of warlike, where casualties are not expected but are more likely to occur than peacetime operations.100 Examples include peacekeeping, mine clearance, and overseas disaster relief. Although they are usually specifically assigned to such operations, ships already at sea only need a single wheel order to execute being reassigned from their current peacetime mission(s).101
Since 1990, Navy has executed several disaster relief operations,102 participated in the maritime campaign to enforce UN sanctions against Iraq,103 and contributed to peace operations in Bougainville104 and the Solomon Islands.105 It also undertook mine clearance operations after the 1991 Gulf War, while continuing to assist with WWII-era explosive ordnance disposal in the south Pacific.106 Navy also prepared to conduct several non-combatant evacuation operations.107
Warlike Operations. Although warlike operations vary in intensity and type, they all involve one or more armed adversaries, and authorisation to apply force in pursuit of specific military objectives. Unlike operations other than war, casualties are expected.
Low intensity operations are limited in aim, scope, and area, and usually have only sporadic fighting. Examples since 1990 include the events prior to East Timorese independence in 1999,108 and the US-led coalition for stabilisation and recovery operations in Iraq from 2003 to 2008.109
Higher intensity conflicts remain limited in aim, scope, and area, but are more likely to employ major weapons systems and involve organised combat operations. Recent maritime examples include the 1991110 and 2003 Gulf Wars.111
General war differs from higher intensity conflicts, not so much regarding combat methods or tactical outcomes, but in its much broader aim, scope and area. It is also the rarest but by far the most critical type of conflict. Fortunately, Australia has not experienced a general war since 1945.
Personnel Factors. In order to conduct these operations, AMD states that Navy’s Mission is to fight and win at sea. As its ethos is therefore that of a fighting service, AMD also states that people are the most important factor to this end, because they determine how Navy platforms are used and supported.112
Sailors worldwide share a common fellowship, based on how wind, water and hidden hazards form a common foe that is far more pitiless and deadlier than any human enemy.113 Even alongside, ships must guard against fires, floods and toxic hazards. Peacetime operations can entail just as long and arduous periods of surveillance and patrol as in wartime, except the latter has intermittent sudden bursts of destruction.
Hence even in peacetime, seagoing life differs substantially from that ashore. Beside the normal activities of daily living, it includes daily damage control and casualty exercises, manually handling boats, stores and lines, data console monitoring, and/or working in confined spaces. These activities throughout the day, in multiple climates and sea states, for weeks or months at a time. They all routinely entail negotiating heavy doors and hatches, often while wearing heavy and uncomfortable personal protective equipment.
All Navy members therefore require physical strength, agility, intelligence, and psychological resilience. The latter especially includes patience, and the ability to share confined living and working spaces for long periods.
These factors drive a form of discipline that stems from understanding the behaviour needed in a fighting service, so members can perform sustainably and effectively for long periods despite fatigue and family isolation, interspersed with the strain, shock and fear of maritime combat. They also explain the need for a spirit that does not accept defeat.
Unlike leadership for land and air operations, which form individuals into fighting instruments, seagoing leadership must form their ship’s company and their ship into a single fighting instrument, with which they share the risks.114
Regarding training, AMD states:
“The processes by which men and women are trained for maritime combat involve both individual and collective efforts. The complexities of modern warships and the systems that they carry mean that naval personnel of all ranks and specialisations require above average intelligence and a high level of education from the outset. The provision of quality basic and specialist training on entry is similarly essential, particularly in an era of minimum crewing concepts. Even with increasingly realistic simulators, however, the individual’s training as a sailor will not be completed until after he or she has had first hand seagoing experience”115 [italics added].
Legal Aspects. Australian maritime operations are subject to domestic legislation such as the Defence Act 1903,116 the Defence Force Discipline Act 1982,117 the Sex Discrimination Act 1984,118 the Disability Discrimination Act 1992,119 and the Work Health and Safety Act 2011120. JHC ‘garrison’ health services ashore also comply with the National Health Act 1953,121 and the Health Insurance Act 1973.122
Among other international agreements, Australia is a signatory to the Geneva Conventions and Protocols,123 which is part of the Law of Armed Conflict (LOAC).124
Implications
Figure 11 summarises the composition, distribution and mobility of the Navy workforce.

The ‘Who’. Unlike the aforementioned civilian communities, the fact that Navy is a young workforce population precludes the need for health services such as paediatrics and geriatrics, and reduces (without eliminating) the need for other health services, such as those related to age-related chronic conditions.
Even without deploying however, their relative youth increases the demand for health services related to workplace- and sports-related musculoskeletal injuries, domestic- and workplace-related mental health issues, and risk-taking behaviours such as driving habits, horseplay, and alcohol and other drug use.
Among their anatomical, psychological, and other differences, men and women have their own illness and injury profiles.125 Combined with their relative youth, this affects the nature and severity of their aforementioned medical conditions, and (especially) how and when they present to health staff.126 As most female Navy members are of childbearing age, potential workplace hazards must also be appropriately managed to ensure their health and safety, and that of any unborn children.127
Navy’s recruiting health standards should enable operational capability by ensuring that candidates can perform their expected duties. Some require specific standards: for example, the importance of visual tasks for aircrew means that, compared to other members, they require a higher visual standard. Similar issues pertain to diver and submariner candidates regarding their airway and lung function.
In addition, Navy’s retention health standards facilitate operational capability with respect to personnel enablers such as promotions, courses, career transfers and (sea) postings.
These requirements therefore not only reflect the limited health services available in remote or austere deployed environments, but also the extent to which even their non-deployed normal duties still require excellent health and wellbeing. However, Navy’s high rates of work-related injuries and illnesses (see below) confirms that high health standards alone do not prevent such conditions, if workplace hazards are not properly managed.
Navy’s workplace complexity places higher demands on its health services to return ill and injured members to duty as soon as possible, compared to less complex workforces where backfilling is easier. For example, if a ‘ship-stopper’ crew member is medically landed ashore, their ship cannot sail until they are either fit for sea, or replaced by someone with the same skills. The ensuing impacts on operational capability reinforces the need for all Navy members to be medically, dentally and psychologically employable and deployable.
The relevance of high-turnover workforces firstly pertains to them having generally higher rates of workplace injury and illness than low-turnover workforces.128 In addition, many early Navy / ADF separations occur for medical and other involuntary reasons, which often have major mental health and broader societal implications for ex-serving members.129 The latter highlights why managing long-term service-related illness and injuries after separation must begin at the first point of treatment during their service, as per Butler.
In summary, the PN workforce is young, predominantly male (but with an increasing female population of predominantly childbearing age), very complex, has high turnover, is highly geographically dispersed (even within Australia), and is highly geographically mobile (even without deploying). As they constitute something of a ‘perfect storm’ regarding their risk of workplace illness and injury, these attributes ought to be reflected in an enduring military doctrinal reference for maritime operations, based on an occupational health systems model.
The ‘Where’. The distribution of the Navy workforce throughout Australia means its supporting health services cannot achieve the economies of scale of similarly sized co-located populations. Furthermore, locations such as Darwin and Cairns have limited access to many specialist health services that are more readily available in southern Australia’s major urban centres.
Navy’s minimum crewing policy for Fleet units means that non-deployable seagoing members must be landed ashore. This contrasts with Army and Air Force, whose non-deployable personnel can remain posted to their unit unless it actually deploys.130 The ensuing ‘crash’ postings of erstwhile shore-based members further reinforces their need to be as medically, dentally and psychologically deployable as those already at sea.
Yet at present, health technical control for Navy’s 4700 seagoing members is currently divided among:
* Six regionally-organised JHC ‘garrison’ health services, when alongside within Australia. Access to these services is limited to however long (or briefly) their ship is alongside, amid multiple competing workplace, personal and other commitments before sailing again.
* JOC when force-assigned (17.0 per cent of all seagoing Navy members), except when alongside in Australia.
* Fleet Health Division at Fleet Headquarters (the remaining 83.0 per cent), except when alongside in Australia.
In addition, health technical control for Navy’s 9,300 shore-based personnel is also divided among JHC’s ‘garrison’ health services.
As personnel move among ships and shore establishments (Figures 4 and 10), the resulting difficulties maintaining continuity of care impedes patient safety. It also precludes consistent shore-based maritime operational health expertise and support, especially with respect to assessing each member’s medical, dental and psychological suitability for sea.131
Hence, a future military doctrinal reference should indicate that the operational need for consistency of health services between (for example) Kuttabul, Cairns, and Stirling outweighs the non-operational treatment-service-driven impetus for uniformity between (for example) Kuttabul (mostly Navy), Holsworthy (mostly Army) and Richmond (mostly Air Force).
From an occupational health systems perspective, this requirement implies that the health services that support PN members ashore and ships alongside should be functionally rather than regionally organised.
The ‘Why’. Australia’s strategic geography explains why Australia has a Navy for reasons beyond territorial defence. It also means that, unlike many other navies (as well as Army and Air Force), its Navy has up to 1600 people at sea every day, who may be thousands of kilometres from their homeports and supporting health services. This especially refers to operations south of the Sandison Line,132 where ill and injured members cannot be readily evacuated ashore.133 Even north of the Line, the ADF has only one permanent overseas base within the northern archipelago, which even then can only provide limited maritime health support.134 While the ADF has deployable land health units,135 they do not normally support peacetime maritime operations. Meanwhile, many overseas military and civilian health services cannot meet even their own population needs.136
Hence, Navy must be able to treat ill and injured members at sea: not only to alleviate their suffering but also to maintain operational capability, by returning them to duty as soon as possible, and/or reducing the need to evacuate them ashore. This requirement drives the need for a risk management approach by health staff afloat and ashore that keeps members at sea where it is clinically and operationally appropriate. Navy’s workforce mobility and complexity also explains why this approach must be applied to all personnel.
AMD indicates that, all else being equal, health staff with seagoing experience can better apply such an approach than those without.137 Navy health staff therefore should not only provide seagoing treatment services as an end unto itself: they should also enable operational capability by keeping people at sea who otherwise would be landed for treatment, while additionally gaining seagoing experience as military health service enablers with respect to their subsequent clinical duties ashore.
These considerations should all form part of an enduring military doctrinal reference.
The ‘How’. Health threats for peacetime maritime operations are generally limited to those associated with simply being at sea. Their health support therefore only entails considering ship’s company demographics, where and how long they are at sea, and the nature of the operation(s) they are conducting.
Maritime health support for operations other than war overlaps with peacetime operations but typically requires targeted augmentation, usually in response to a particular incident. However, the initial response may still have to employ each ship’s organic health assets. Maritime health support for warlike operations likewise overlaps with operations other than war, except targeted augmentation is required in anticipation of BCas as well as DNBI.
Figure 10 indicates that the scope of the health services that enable maritime operations is far broader than deployable treatment services for battle casualties (BCas), or even seagoing treatment services in general. It also indicates that, despite their often essential requirements for health support, amphibious operations are only one type of maritime operation among many others that also require such support.
While civilians have important (often essential) health roles, the importance of people to Navy’s fighting ethos highlights how maritime health support must be underpinned by uniformed health staff under service discipline. Their contributions to morale per AMD include meeting every Navy member’s expectation that they will be there if they are ill or injured,138 while facilitating the balance between their needs and those of their ship, consistent with Navy’s Values and Signature Behaviours.139
Uniformed health staff are also required to conduct leadership roles such as providing health advice to commanders, and managing their maritime health assets.140 Navy health staff who perform such roles therefore need escalating levels of military and population health (not just primary care treatment) expertise as part of their career progression.
Among other obligations, LOAC requires the health assets that support these operations to be declared as such and marked with a protective emblem. This is problematic for Navy because its platforms can only provide non-declared organic health support.141 It also affects health staff such as minehunter and submarine medics, who perform combatant roles in addition to their duties as medics.
In summary, the essential role of people to Navy’s Mission highlights the need to ensure their health and wellbeing. While Australia’s maritime operations are conducted jointly, the extent to which its strategic geographic considerations are unique to Navy operations must be reflected by its supporting health services. This especially refers to the extent to which the workplace activities conducted by all Navy members are elementally shaped by the environment in which those who happen to be at sea at a particular time perform their duties. These considerations should be incorporated into an enduring military doctrinal reference for maritime health support.
Maritime health services: the ‘What’
Having ascertained the attributes of the target population per Figure 2, the health service missions to support maritime operations per Butler should be conducted via the following health functions and roles per Figure 1.
Operational Health Support. As previously indicated, military health services have three missions, with one always taking priority depending on circumstances:
* Providing targeted treatment services based on the demographics of the relevant population (whether deployed or not), their location, the operations they conduct, and how they conduct them.
* Enabling operational capability by maintaining the health of deployed and non-deployed members, managing the timely return of ill and injured members to normal duties, and if this is not possible, facilitating their timely disposition elsewhere.
* Facilitating their eventual separation from the ADF regarding their long-term service-related illnesses and injuries from their first point of treatment, including while deployed.
The geographic mobility and complexity of the Navy workforce means the health planners responsible for Fleet units (whether at sea or alongside) require a comprehensive grasp of:
* How to best employ their allocated FiCs to conduct all the enabling military health functions and roles per Figure 1, in support of maritime operations.
* Vice versa, ie how the maritime environment and/or FiC shortfalls affect the performance of these military health functions and roles.
Shipboard space limitations (see below) mean that unlike their land counterparts, maritime health planners cannot ‘work forward’ from a casualty estimate to ascertain what health support is required. Rather, they first have to consider each ship’s health capabilities, and ‘work backwards’ to ascertain what kind and how many casualties can be managed.
As previously indicated, AMD indicates these considerations are best managed by health staff with actual seagoing experience.142
Casualty Evacuation. Although Fleet units deployed thousands of kilometres from their home port must be medically self-sustaining per above, they still require the ability to evacuate the right casualties, at the right time, in the right order, with the right level of en-route care, to the right health facilities.
Among other skills (in particular, a complete understanding of the capabilities and limitations of the allocated platforms), casualty evacuation health staff require clinical trauma and mental health expertise, while moving casualties by air needs a high level of aviation medicine awareness. Fixed-wing aeromedical evacuation (AME) is a recognised core air mobility role of the Air Force health services.143
HA/DR. While maritime HA/DR is an effective ‘soft power’ means of advancing national objectives,144 this paper has explained why treatment services for military personnel differ from those for civilian women, children, elderly and disabled. Lack of predictability means that HA/DR response times are usually far shorter than for other military operations,145 while rather unusually, HA/DR health units may be the force being supported by other arms, instead of acting as a supporting arm for a deployed force.146 Once deployed, HA/DR health support also usually demands close interaction with multiple non-government organisations and other civilian agencies.147
Military Medicine Capabilities. Military medicine capabilities support operational assets such as submarines, combat aircraft (including helicopters), diving capabilities (such as mine disposal and underwater battle damage repair), and Chemical, Biological, Radiological and Nuclear (CBRN) defence.148
As of 01 Mar 2018, 2,439 Navy members (17.4 per cent) were either aircrew, divers, submariners, joint battlespace aircraft controllers or parachutists. While they have the same health support requirements as other Navy members, the additional physiological and human factors hazards associated with their duties necessitate dedicated health services, with the following amended missions:
* Targeted health services that reflect the physiological and other hazards inherent to these workforces. For example, divers and submariners require deployable emergency hyperbaric treatment services, the latter including the ability to manage multiple casualties from a survivable submarine accident. Similar considerations pertain to CBRN threats.
* With respect to enabling operational capability, their scarce (and expensive) skills drive the need to return ill and injured members to their normal duties as soon as possible under specific medical supervision.
* Facilitating their eventual separation as for other Navy members, albeit for specific medical conditions related to their duties.
Health Suitability for Employment and Deployment.149 Navy members may be posted to sea for up to two years, during which time they are likely to undertake several deployments. Many also undergo multiple such postings during their career. The fact that the shipboard environment is more self-contained than ashore means that, unlike Army and Air Force, assessing suitability for sea for Navy members can be an ‘all-hazards’ approach based on each seagoing posting, rather than each deployment they undertake.150
It is well-understood that deployed medically, dentally or psychologically unsuitable members compromises operational capability and pose a risk to themselves if they cannot receive the care they need.151 IN addition, evacuating members with known pre-existing conditions threatens the safety of other members, and wastes resources that should otherwise be employed achieving the mission.152
What is less-well-understood however, is that blocking members from deploying unnecessarily also compromises operational capability. Besides limiting or precluding current operations in the short term (for example ‘ship-stopper’ crew members), it also impedes medium term operational capability by delaying or blocking their career progression, which can result in eminently avoidable longer-term retention issues among members with scarce or hard-to-replace skills.
An added complication is that the overzealous medical separation of members who simply need more time before resuming their normal duties has similar effects on medium- and longer-term Navy operational capability.
Assessing health-related suitability for military service must therefore begin at recruitment, and continue as a day-to-day military health function until separation. As previously indicated, this demands a risk management approach153 with respect to:
* The effect of each member’s medical condition(s) on their ability to perform their normal duties.
* Vice versa, ie the effect of their normal duties on their medical condition(s).
This approach achieves two aims: it facilitates Navy’s duty of care by reducing the risk of further harm;154 and enables Navy operational capability by maximising employment and improved retention in accordance with CN’s imperative. It is also consistent with studies confirming that keeping ill and injured employees in good work maintains their physical, social and psychological health.155
All ADF members with medical restrictions for more than 28 days require a Medical Employment Classification (MEC) Review (Medical Board of Survey for Navy personnel prior to 2000).156 The graph per Figure 12 describes the Medical Category (MEDCAT) status of all Navy members as of 30 Jun 96, while Figure 13 describes the Medical Employment Classification (MEC) status of all Navy members as of 01 Mar 18.
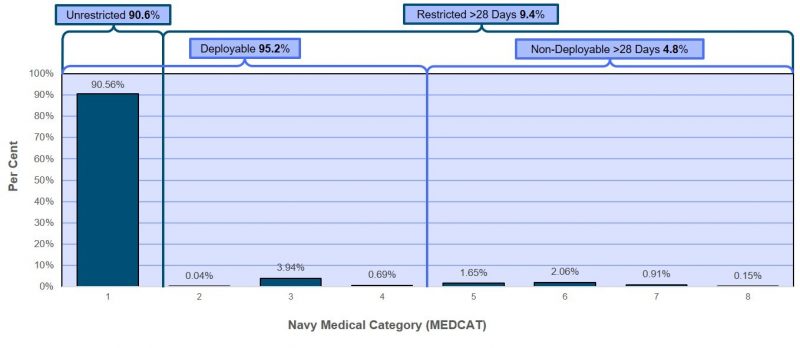
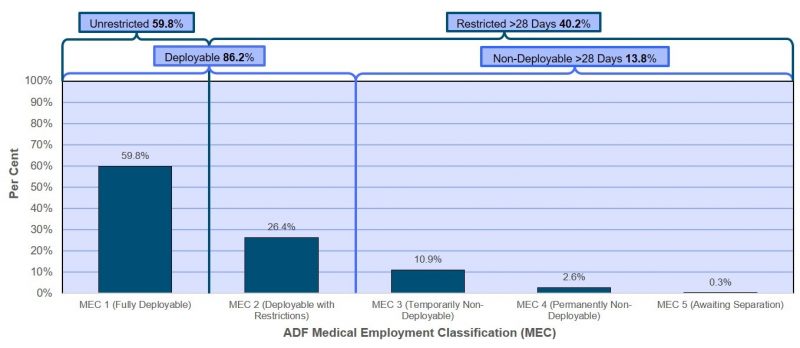
Figures 12 and 13 indicate that the proportion of Navy members deemed not medically suitable for sea for more than 28 days has increased from 4.8 per cent in 1996 to 13.8 per cent in 2018, while those with at least one medical restriction for more than 28 days has increased from 9.4 to 40.2 per cent.
These figures suggest that a significant proportion of Navy members are being made unfit for sea unnecessarily.159 They may also indicate the extent to which CN’s imperative to get more platforms to sea (hence Navy operational capability) is being impeded by the ADF’s current health service delivery model.
Occupational and Environmental Health (OEH). Despite the focus by military planners on weapons that kill or maim, Navy members ashore and afloat can also be exposed to non-operational workplace hazards such as:
* Physical: heat, cold, noise, vibration, and radiation (ionising and non-ionising).
* Chemical: solids, liquids, dusts, fumes, mists and gases.
* Biological: vermin, parasites, protozoa, fungi, bacteria, rickettsia and viruses.
* Ergonomic, in particular personnel / machine interfaces.
* Human factors: shift work / fatigue, and bullying / harassment.
Unlike ashore, these hazards generally remain unchanged at sea, despite ships moving within hours or days between (for example) high- and low-threat operational areas, or between the tropics and sub-Antarctic. Hence, unlike the other Services maritime OEH support should reflect each ship (or even ship class) rather than their location.
Current OEH legislation imposes a duty of care on commanders to minimise exposures to workplace hazards.160 However, the demands on them to achieve their mission(s), and the fact that junior ADF members lack many of the protections provided by unions and other employee organisations, have led to several high-profile failures to ensure their health and wellbeing.161 The ADF’s workplace injury and illness rates (see below) suggests this continues regarding lower-profile yet common musculoskeletal and mental health conditions.
The ADF appears unique in that unlike civilian employers, neither JHC nor the Defence Work Health and Safety Branch (DWHSB) collect or report Lost Time from [workplace] Injury Frequency Rate (LTIFR) data. Neither do they record or report restricted duties data, or identify the ensuing treatment care costs.
Rather, unlike most civilian employers that provide employee health care, the ADF’s health services cannot at present accurately ascertain how many medical presentations are work-related.162 For example, JHC clinical records routinely document patient details such as their Service and rank but not their rate (Navy), corps (Army) or mustering (Air Force) that indicate the jobs they perform.163
Although some – but by no means all – of this information is provided via the DWHSB Work Health and Safety Compensation and Reporting (WHSCAR) System (‘Sentinel’), a recent study indicates that only 11 to 19 per cent of all Army Reserve and Regular work-related injuries and illnesses are being reported.164 Notwithstanding its own reporting systems, it is likely Navy workplace illness and injury reporting rates are also under-reported.
Hence Defence lacks visibility regarding the extent to which operational capability is compromised by its work-related illness and injury rates, because accurate enabling data simply does not exist. Collecting this elementary baseline data at the first point of treatment is essential, not only for compensation eligibility purposes, but also to:
* Monitor the effectiveness of the ADF’s and Navy’s OEH services in enabling operational capability by preventing workplace-related illness and injuries.
* Account for the high health care costs incurred by JHC (see below).
* In addition to eligibility, account for the high compensation and veteran health care costs incurred by DVA (see below).
Health Promotion. Military health promotion programs (HPPs) enhance operational capability by improving personnel functionality in hostile or challenging environments, while reducing preventable illness and injury. Their scope is therefore broader than civilian HPPs designed to prevent long-term illness,165 to include (for example) personal health care, physical fitness, resilience training, fatigue management, heat stress prevention, and combat (sea) survival.166
Successful military HPPs require close engagement by both commanders and their supporting health staff.
Treatment Services. It should be apparent by now that the scope of military health services is far broader than simply providing clinical treatment. Even so, health services that that provide poor clinical care or none at all hardly merit being referred to as such.
Maritime BCas are caused by blade- and club-type weapons, small arms, grenades and other explosive devices, artillery rounds, sea-, land- and air-launched missiles, and sea mines and torpedoes. These can cause penetrating wounds, blunt trauma, blast injuries and/or burns. Nuclear and radiological weapons pose additional threats, as do biological and chemical agents.167 All these threats affect human performance, and can create a range of mental health disorders.168
However, consistent with the relationship between BCas and Disease and Non-Battle Injury (DNBI) rates throughout military history, the overwhelming majority of clinical presentations are for DNBI.169 Seagoing DNBI presentations are generally comparable to those in the base setting, apart from additional cases caused by operational workplace health hazards afloat and ashore,170 especially in the northern archipelago and south Pacific.171
It should also be noted that shipboard space constraints intensify weapon effects, resulting in multiple BCas of generally comparable type and severity.172 These constraints also pose major challenges for DNBI infectious disease prevention and control.173
As previously noted, the ADF lacks visibility regarding the extent to which its work-related DNBI rates are compromising operational capability. Even so, a 2009 study of DVA compensation claims for Chondromalacia Patellae (CMP), a painful degenerative condition of the patella (kneecap), indicated that the incidence of this condition alone within Navy was 0.33 per cent per year, most of which developed in the first years of service.174 Noting their median duration of service is seven years, every Navy member therefore has a 2.31 per cent likelihood of developing compensable CMP during their career. Furthermore, if CMP is one of the five most common musculoskeletal disorders in Navy, and if their incidence rates are comparable, 1.65 per cent of its workforce (231 new cases, or one FFG crew) would sustain compensable musculoskeletal injuries alone every year.
Moreover, Australia had about 741,300 current and ex-serving ADF members in 2017-18, including 150,200 with peacetime-only service. Of the total, 190,967 (29.8 per cent) received health services from DVA for service-related conditions (Gold and White Cards),175 costing $5.3 billion, or $7,149 per member ($27,753 per member with an accepted claim).176
By comparison, the average per capita cost of civilian health care in 2016-17 was $7,411.177 In other words, the per capita cost of treating service-related injuries and illness alone to DVA, is about the same as that expended on the general population, despite the latter including high-cost non-workforce groups such as children, the elderly and the disabled.
To this can be added another $7.4 billion spent by DVA on the following non-treatment compensation and disability services:178
* 85,811 current and ex-ADF members received a disability pension per the Veteran’s Entitlements Act 1986 (VEA).
* 5,767 received a weekly incapacity payment per the Safety Rehabilitation and Compensation (Defence-Related Claims) Act 1988 (DRCA) or the Military Rehabilitation and Compensation Act 2004 (MRCA).
* Between 12,414 and 26,564 current and ex-ADF members received one-off permanent impairment payments from either the DRCA, the MRCA, or both.179
Hence, between 140 and 159 per 1000 current and ex-ADF members received some form of compensation or disability payment for at least one service-related medical condition, at a per capita cost (additional to the treatment costs above) of $9,982 (or at least $62,636 per member with an accepted claim).
Comparing this data with civilian worker’s compensation claim data is not straightforward, noting that the latter are subject to multiple federal, state and territory jurisdictions. For example, Safe Work Australia states that Australia had 10.6 million employees in 2012-13,180 while the Work-Related Injuries Survey infers there were 12.4 million employees.181
Even so, the most recent SafeWork Australia data indicates that the median cost182 of civilian claims in 2012-13 was $8,900,183 while the Work-Related Injuries Survey showed the estimated total cost was $61.8 billion (4.1% of GDP),184 or $5,000 to $5,800 per employee.
The Work-Related Injuries Survey also indicated that during that time, an estimated 531,800 workers (4.3%) had experienced a work-related incident. 348,600 workers did not receive compensation, either because no application was made, or the application was rejected.185 Of the remaining 183,200 workers, Safe Work Australia showed that:
* 117,815 were for serious worker’s compensation claims (requiring a work absence of one working week or more), or 11.1 claims per 1000 employees.186
* Employees working as labourers had the worst serious claim incidence rate of all civilian occupations (27.0 per 1000 employees).
Hence, the current ADF compensation claim incidence rate could be 12 times the average civilian serious claim incidence rate, and five times the worst civilian serious claim incidence rate. Moreover, the per capita cost of compensation for current and ex-ADF members could be twice the Safe Work Australia median civilian rate and the average Work-related Injuries Survey civilian rates.
The magnitude of these disparities makes it unlikely that they can be ascribed to different compensation eligibility criteria or entitlements. They also suggest the possible extent to which the ADF’s high health costs are not caused by over-servicing,187 but by its health services providing care for generally preventable workplace illnesses and injuries, as an over-employed ‘Ambulance Down in the Valley’.188
Regarding differences between the medical conditions seen by Defence health staff compared to the civilian community, the ADF’s Health Surveillance System (EpiTrack) 189 showed that in 2007-08 and 2008-09, the five most common medical conditions were:
* Injuries and musculoskeletal disorders.
* Respiratory tract conditions.
* Skin conditions.
* ‘Ill-defined’ (but often ascribed to mental health) conditions.
* Ear, nose and throat disorders.
EpiTrack data also showed that the five most common medical conditions resulting in sick leave at that time were:
* Injuries and musculoskeletal disorders.
* Respiratory tract conditions.
* Mental health disorders.
* Stress reactions.
* ‘Ill-defined’ conditions.
* Intestinal infectious disease.190
By comparison, the five most common civilian clinical presentations in 2013 were:
* Hypertension.
* (Childhood) immunisations,
* Upper Respiratory Tract Infections.
* (Non-work-related) depression.
* Diabetes.191
The EpiTrack data shows how the medical conditions among ADF members differ from those in the civilian community, in particular musculoskeletal and mental health conditions among the former, many of which are likely to be work-related.
Furthermore, Figure 14 lists the 15 most frequently claimed conditions under the VEA, which constituted 61.5% of all such claims in 2015.192 This indicates that at least 22 per cent of VEA claims were for musculoskeletal conditions, while at least another nine per cent (including alcohol use disorder) were for mental health issues. Other conditions for which a relatively straightforward relationship with ADF employment exists include hearing disorders secondary to workplace noise (16 per cent), skin disorders secondary to sun exposure (seven per cent), and a small number of eye disorders secondary to ultraviolet-light exposure (e.g. arc welding).

It therefore seems possible that, pending better data:
* About 30-40 per cent of ADF clinical presentations are for generally preventable musculoskeletal injuries. Perhaps half are work-related (typically related to manual handling or slips / trips / falls); the remainder are most likely sports-related.
* Another 30-40 per cent of ‘garrison’ clinical presentations are for generally preventable work-related mental health issues. Perhaps half lack psychological robustness for whom the ADF has been a poor career choice; the remainder are quite likely to be just as psychologically robust as other ADF members, but are not coping with excessively demanding or otherwise dysfunctional workplaces or personnel management practices.
Hence, perhaps half of all ‘garrison’ primary care presentations are for work-related conditions. This estimate should be compared with 2013-14 data indicating that only 2.4 per cent of civilian general practitioner presentations were work-related.193
While admittedly imperfect, these figures indicate the need to improve ADF / Navy OEH hazard management, with an added emphasis on prevention before treatment. They also validate this paper’s assertion that a future military health doctrine for maritime operations must be based on an occupational health systems model.
Maritime health service FiCs
The health services that support maritime operations need the following FiCs, in order to conduct the aforementioned functions and roles that enable their missions per Butler.
Command and Management. Health services that support (in this case maritime) operations require structured health command and administrative systems that interact closely with the relevant commanders ashore and afloat. As previously indicated, the uniformed health staff who conduct the ensuing leadership roles need escalating levels of military and population health expertise, as part of their career progression.
Organisation. This paper has described why the health units that support maritime operations must be organised to reflect all of the attributes of the entire full-time Navy workforce (deployed and non-deployed), whose involvement in such operations are inherent to their normal duties.
This paper has also referred to the location, distance, shipboard space and other constraints on health support. These compel a scaled approach to maritime health services, the organisation of which (again) demands a risk management approach, based on an occupational health systems model that is (again) best achieved by health staff with actual seagoing experience.
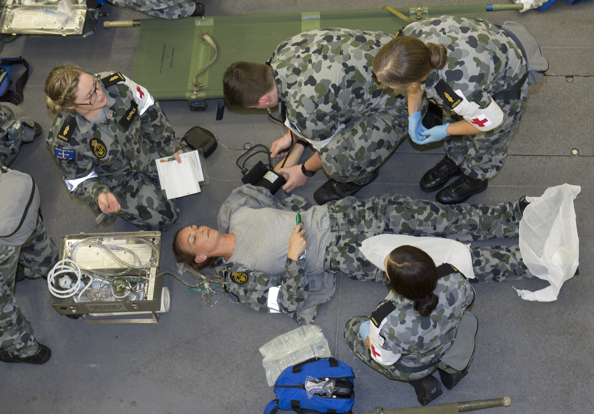
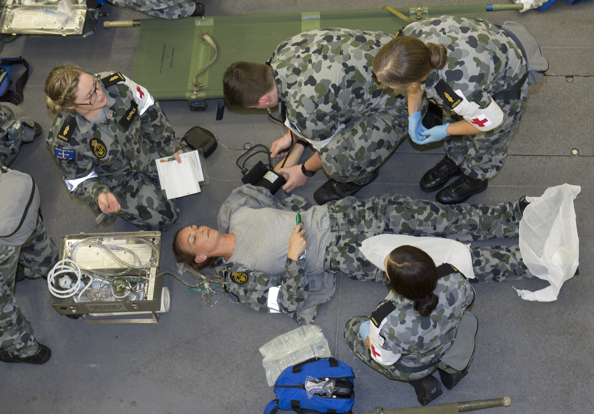
Personnel. This paper has explained how Navy’s ethos as a disciplined fighting service means its uniformed health personnel must be the bedrock of maritime health support.
Health staff recruiting and entry training should reflect their initial role of providing care within their scope of clinical practice, in at times exceptionally remote and/or austere situations where casualty evacuation may be delayed. This refers to the skills, knowledge, expertise and currency to manage (not just treat):
* clinical conditions that are usually only encountered overseas,194 and
* being beset by mass BCas and/or DNBI.
Moreover, Navy’s minimum crewing policy will continue to drive multiskilling for:
* Dedicated health staff aboard major Fleet units, with respect to their non-health whole-of-ship obligations.
* Non-health staff aboard major Fleet units who assist dedicated health staff.
* Non-health staff aboard minor war vessels without a dedicated health staff member who nevertheless are still required to provide health care.
Collective Training. Like the rest of Navy, seagoing health staff not only must be mission-ready as individuals, but also as part of their ship’s medical department and their ship’s company per AMD. Hence, their collective training must shape their clinical and military skills into a health team, for broader integration into the Fleet unit in which they serve. This requirement therefore suggests that all seagoing-specific health support should be provided by Navy health staff.
Civilian health industry support. Notwithstanding the previous assertion that uniformed health personnel must be the bedrock of maritime health support, health support for such operations is complicated by the extent to which the technological health advances over recent decades have led to increasing levels of specialisation.195 As this precludes Navy and the broader ADF from providing the full range of DNBI and BCas health services organically, their reliance on the clinical skills and expertise that is only available from the civilian health system ashore can be expected to increase. Even so, Navy Reserve health staff have an essential bridging role between the civilian, deployed and non-deployed settings.196
Other FiCs. These include the relevant:
* Seagoing health facilities (dedicated and non-dedicated).
* Supply (including medical equipment and pharmacy consumables).
* Major systems (in particular health information technology).
* Support from the Fleet unit(s) whose operations they are enabling in order to function (such as first aid parties, patient catering, and bed linen).
As previously indicated, shipboard constraints on all of these FiCs further compel a scaled approach to maritime health support, based on risk management.
Conclusion
This paper describes why the functions and roles of Navy’s supporting health services entail more than simply delivering clinical care, or only considering the non-clinical logistic and administrative aspects of establishing and operating deployable health facilities. It seems likely that longstanding misperceptions to this end have had profound adverse impacts on ADF and Navy operational capability.
Ascertaining what health services are required for PN personnel ashore and afloat should begin with their demographics, in particular their higher rates of musculoskeletal injuries, and health issues compared to civilians. Ascertaining the extent to which these are work-related demands improved data collection at the first point of treatment.
This paper explains why the Navy workforce requires a surprisingly broad range of health services ashore and afloat compared to equivalent-sized civilian communities. These should reflect their higher rates of non-operational workplace-related musculoskeletal conditions and mental health issues, as well as operational DNBI and BCas when required.
Yet, the distribution and mobility of PN personnel throughout Australia not only affects how they receive these services. Besides creating an exceptionally demanding continuity of health care setting, they also cause or exacerbate adverse health effects in their own right (particularly their mental health). These attributes are further exacerbated by Navy’s workforce complexity.
Furthermore, unlike the other services Navy routinely deploys hundreds of members at a time up to thousands of kilometres from its major bases and their associated health services. This drives the need for a wide range of scalable clinical services in remote and/or austere locations, where casualty evacuation may be delayed. They also explain why Navy’s base health services must be seamlessly linked, not only to those afloat, but also to non-Navy health service providers throughout Australia, including the civilian health system.
Besides treatment services, Defence health staff must also ensure all Navy members are medically, dentally and psychologically suitable for sea, and if this not possible, either enable their return to normal duties as soon as possible, or facilitate their timely landing ashore and/or transition to the civilian community. Determining how their patients’ duties affects their health, and how their health limits or prevents them from performing their duties, requires a risk management approach that is best achieved using an occupation health systems model, by health staff with (in this case) actual seagoing experience.
Assessing suitability for sea for Navy members should be an ‘all-hazards’ approach based on each seagoing posting, rather than each deployment they undertake. Likewise, maritime OEH support should reflect each ship (or even ship class) rather than each ship’s location.
Notwithstanding the at times essential contribution of civilian health providers, Navy’s ethos as a disciplined fighting service means its uniformed health personnel must be the bedrock of maritime health support. Their contributions to morale include meeting the expectation that whatever happens, they will be there for ill or injured Navy members, while employing a risk management approach to balancing their needs with the Service.
This paper has described some elements of, an enduring military doctrinal reference as to how health support for Australian maritime operations should be directed, mounted, commanded, conducted, sustained and concluded, in support of CN’s imperative for more platforms at sea. Its intent must extend beyond providing treatment, to also enabling maritime operational capability with respect to each member’s medical, dental and psychological suitability for deployment, and facilitating their eventual return to the civilian community with respect to their long-term work-related illnesses and injuries.
It should also drive a new primary mission for the Navy Health Services:
Enabling Navy’s Mission (to fight and win at sea), by optimising the health and wellbeing of its personnel through constant care.
____________________________________________________

*Dr Neil Westphalen (email: neil.westphalen@bigpond.com) graduated from Adelaide University in 1985 and joined the RAN in 1987. He is a RAN Staff Course graduate and a Fellow of the Royal Australian College of General Practitioners, the Australasian Faculty of Occupational and Environmental Medicine, and the Australasian College of Aerospace Medicine. He also holds a Diploma of Aviation Medicine and a Master of Public Health.
His seagoing service includes HMA Ships Swan, Stalwart, Success, Sydney, Perthand Choules, while his deployments include DAMASK VII, RIMPAC 96, TANAGER, RELEX II, GEMSBOK, TALISMAN SABRE 07, RENDERSAFE 14, SEA RAIDER 15, KAKADU 16 and SEA HORIZON 17. His service ashore includes clinical roles at Cerberus, Penguin, Kuttabul, Albatrossand Stirling, and staff positions as Director Health at the then Headquarters Australian Theatre (now Joint operations Command), Director Navy Occupational and Environmental Health, Director of Navy Health, Joint Health Command Staff Officer One Medical Employment Classification Advisory and Review Services and Fleet Medical Officer, before transferring to the Active Reserve in 2016.
Disclaimer: The author used some of the information in this article to lead a Royal Australasian College of Physicians (RACP) submission to a Productivity Commission inquiry regarding veteran’s rehabilitation and compensation.[i]However, the views expressed in this article are his alone, and do not represent those of the RACP, the RAN or any other organisations mentioned.